“I was one of the first people in Poland who got an insulin pump in 2000. And it completely changed my life,” says Dr Kate Gajewska, a diabetes specialist now living in Ireland who herself has diabetes.
In the 1980s, she says, the average person with diabetes would develop complications and would die quite soon. “We were just blind in terms of diabetes management and control.”
But her insulin pump, though, now means she doesn’t have to “eat the same meal at the same time like I did the 12 years before”. Instead, she can deliver insulin into her bloodstream straight away before meals and calculate different doses.
“Across my lifespan there are so many tech game changes” for living with diabetes, recalls Dr Gajewska, who is now clinical director for research and advocacy at Diabetes Ireland. Her first blood glucose metre, for instance, “also changed my life entirely”.
Then came continuous glucose monitoring, “another gamechanger, checking every three or four hours, so finally you have everything on a graph, when you’re going low, high, it gives you alarms and contexts”. For diabetes, technology is “the cure, it’s what I believe in,” says Dr Gajewska.
Important new innovations include work by Fada Medical in Galway, a spin-out combining the efforts of Professor Garry Duffy and Dr Eimear Dolan at the University of Galway, and Professor Ellen Roche at MIT.
One of the most critical parts of an insulin pump is the cannula (called an infusion set cannula, or ISC), a small tube that connects the pump with a person’s subcutaneous tissue. An ISC today usually lasts two to three days before it has to be changed. The Fada researchers have (the clue’s in the name) found a way to lengthen this, to up to 30 days. It is clear too, at the moment, where all this technology is heading.
“The beauty of medtech innovation in diabetes is it has a clear global focus – everyone is working towards an artificial pancreas,” says Dr Aleksandar Petrovic, a Basel-based senior global medtech principal at consultancy Iqvia.
The holy grail of an artificial pancreas
But it’s also clear it isn’t quite yet there. Globally, 537million adults live with diabetes. In Ireland, it is the most chronic condition for people between 45 and 75. It is the most expensive chronic disease, costing $327 billion a year in America alone.
An artificial pancreas would combine continuous glucose monitoring, an insulin delivery device, and an algorithm that uses the glucose information to make insulin delivery decisions in a fully automatic way, without input from users.
“These are trials really,” says Dr Gajewska. These include trials in the NHS since April 2022. Instead, most systems are still “hybrid closed loops,” where you have to tell the system if you “exercise, or are insulin resistant from stress, or eating a high fat meal, or illness,” says Melissa Holloway, who is both diabetic and founder of a London diabetes start-up.
A continuous closed loop system could check someone’s blood sugar up to every couple of minutes, and deliver frequent smaller doses of insulin throughout the day as needed. And, points out Dr Gajewska, smartphones can already tell if you’re exercising, or crashing on your sofa. So using this information in making insulin delivery decisions should be an easy enough task.
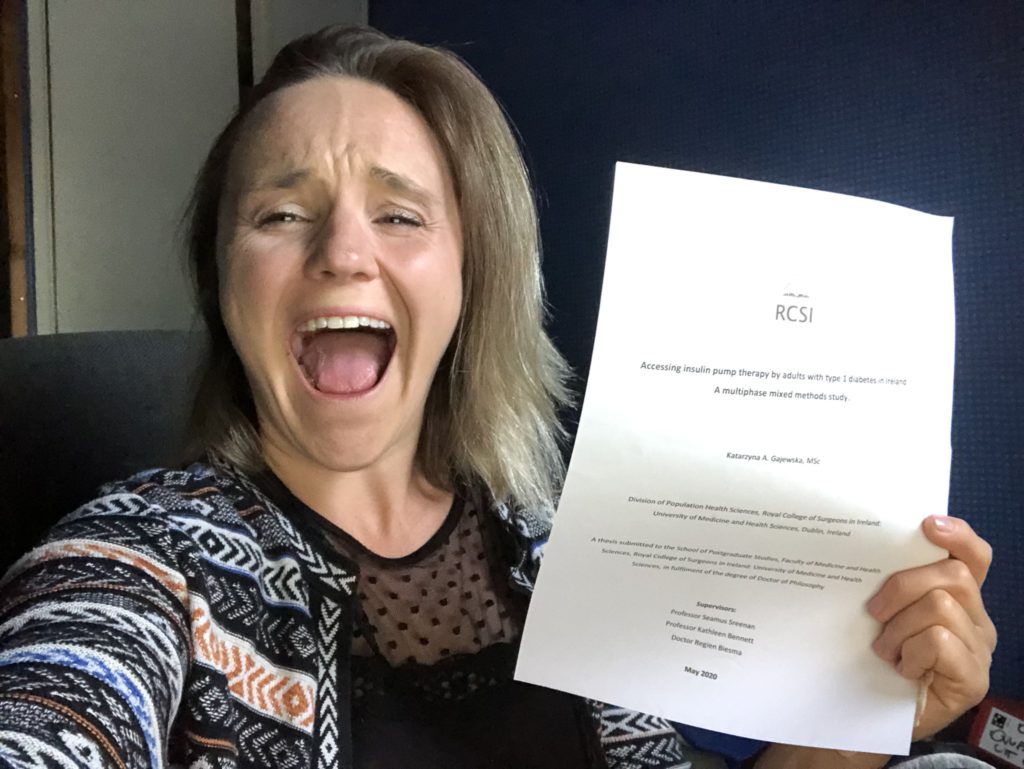
Dr Kate Gajewska
Insulin pump uptake
Uptake in Ireland of insulin pumps is astonishingly low, says Dr Gajewska, whose doctorate was on precisely that topic. In Germany, 40 per cent of adults with diabetes use insulin pumps. In the UK, this is even higher, at 50 per cent. But in Ireland, the corresponding figure is only seven per cent. The main barrier, she says, is health professionals’ attitudes.
If you have a health care professional who is not technologically focussed, as a diabetes patient “you will hear no – ‘we have no capacity, no trained nurses, no dieticians, to learn how to use an insulin pump'”.
One third of clinics in Ireland are not even offering follow up care for people who have pumps, she says, “which I think is disgraceful, pumps are a modern technology, it’s been there 20 years”.
There is public reimbursement for adults for three continuous glucose metres in Ireland, but not for the FreeStyle Libra sensor, a commonly used one.
“Ireland is the only one country in Europe where Libra is not available to people” for free, “the fun thing is Abbott, the company producing it has their main office in Ireland,” she says.
Do it yourself better
Commercial devices tend to talk to less well to other commercial devices, which is one reason many people with diabetes use DIY solutions.
“I can’t, for example, now deliver insulin from my iPhone, or Apple Watch,” Dr Gajewska says. “But when I was using a DIY system, I could just click a few buttons on my watch and I was delivering insulin.” About 30,000 people with Type 1 diabetes use an opensource artificial pancreas system, according to a February 2023 study pre-print in the Lancet.
“I’m still doing DIY because after four and a half years, I know more about my priorities and daily management,” says Ms Holloway, whose own start-up SmartStart Health is developing a continuous glucose monitoring app.
“And I’m looking for specific features to be launched and certain technologies to come to market, that aren’t quite ready yet, but the gap is closing,” she says.
These include “convenience factors and a bit of tech,” she explains. “I want to be able to control the system with my iPhone, while so far, the tech on the market is android only.” And while some next generation commercial technology will enable them to target a slightly tighter target, “it’s still not the tight target I can target and set with my DIY setup,” she adds.
The average time people using a DIY open-source system spent in their target glycemic range increased from 64 per cent beforehand to 80 per cent with the DIY system, said researchers from BCDiabetes in Vancouver in the Lancet preprint.
Researchers at Cambridge found even more startling results in January, with DIY patients spending twice as much time within the ideal blood glucose level range compared with in the control group.

Melissa Holloway Picture: juliantse.com
Watch this space
It’s an exciting time for new developments in diabetes generally. Screening is important, since type 1 diabetes needs to be diagnosed quickly to avoid life-threatening complications. Currently, over a quarter of children aren’t diagnosed with type 1 diabetes until they are in the serious and often life threatening condition called diabetic ketoacidosis (or DKA).
A new trial screening programme in the UK called ELSA can screen children for autoantibodies, signs in the blood that the immune attack has started. People with two or more different autoantibodies have an 85 per cent chance of developing type 1 diabetes within 15 years, and it’s almost certain that they will develop it at some point in their lifetime.
So knowing someone is about to develop type 1 diabetes means they can have a softer landing into a life with diabetes, and manage the condition from the start.
And the world’s first ever immunotherapy for type 1 diabetes was approved by the FDA in the US late last year. “It’s the biggest breakthrough for type 1 since the discovery of insulin, just over 100 years ago,” says Fiona McLoone, a recent Trinity College Dublin graduate working as research officer at Diabetes UK.
This drug, called Teplizumab, is called a monoclonal antibody, whose job is to hunt down and weaken the killer immune cells responsible for destroying insulin-making beta cells.
This helps to protect some beta cells from the immune attack and means people can keep on making their own insulin for longer. It can slow the development of type 1 diabetes and also delay a diagnosis, by up to three years, in people at high risk of the condition.
And as people living with diabetes get access to these life-changing new technologies, the fact many have them have been hacking their own bodies will make them an unusually educated and receptive audience.
“When you think of your own body as a science experiment, you get feedback, and in that feedback loop you can make more informed decisions,” adds Melissa Holloway.






